Why Treatment and Documentation Should Never Be Separate
How clinical reasoning connects what you do in treatment to what you write in your notes
One of the most common struggles for OT students and clinicians is knowing what to do with a patient but not knowing how to document it clearly and defensibly. Treatment and documentation are often treated as two separate tasks, when in reality, they are part of the same clinical process.
Treatment reflects your clinical reasoning. Documentation should reflect that same reasoning in written form. When those two drift apart, notes become vague, repetitive, or focused on tasks rather than skilled intervention.
Consider a common inpatient rehab scenario. A client is working on grooming at the sink following a stroke. During the session, the OT emphasizes standing tolerance, one-handed task performance, and sequencing because of hemiparesis and impaired balance.
If the note simply states, “Patient completed grooming at sink with mod A,” the intervention looks task-based and generic.
But when documentation mirrors the treatment decision-making, the clinical skill becomes visible. A stronger entry might look like:
“Patient completed grooming in standing to address dynamic balance and unilateral upper extremity use secondary to left hemiparesis, requiring mod A for postural stability and task sequencing to improve functional independence with self-care.”
Here, the treatment choice (standing grooming) and the documentation are telling the same clinical story.
In real-world practice, clinicians are expected to demonstrate skill through both intervention and written justification. Productivity demands, varying facility standards, and limited time make it easy for documentation to become a rushed afterthought. Over time, this creates a pattern of writing notes that describe what was done without clearly communicating why it was done or how it supported occupational performance.
This gap becomes especially clear in home health. An OT may address fall risk by working with a client in the kitchen, focusing on weight shifting, visual scanning, and safe item retrieval from cabinets. If the note only reports that a “kitchen task was completed,” the skilled reasoning behind the intervention is lost.
When treatment and documentation are aligned, the purpose of the task is made explicit. A stronger note might read:
“Engaged patient in kitchen-based task requiring weight shifting and visual scanning to address balance deficits and reduce fall risk during meal preparation, with verbal cues provided for safe item retrieval and environmental awareness.”
Now the task is no longer just “kitchen activity”—it is clearly tied to safety, function, and clinical reasoning.
Skilled OT practice depends on the ability to link client needs, intervention choices, and functional outcomes. When documentation is separated from treatment, that link weakens. Notes may still be completed, but the clinical story becomes unclear. This is often where clinicians begin to feel uncertain about whether their documentation truly reflects skilled care.
The same pattern appears in outpatient settings. A client working toward returning to work may perform therapeutic exercises for upper extremity strength. If the note only states, “Completed theraband exercises,” the intervention looks generic and interchangeable.
When documentation reflects the treatment intent, the intervention becomes purposeful. For example:
“Patient performed progressive resistive upper extremity exercises to improve grip strength and endurance required for sustained work-related lifting tasks, with rest breaks incorporated to address activity tolerance limitations.”
In this case, the exercise is no longer just exercise—it is directly connected to occupational performance.
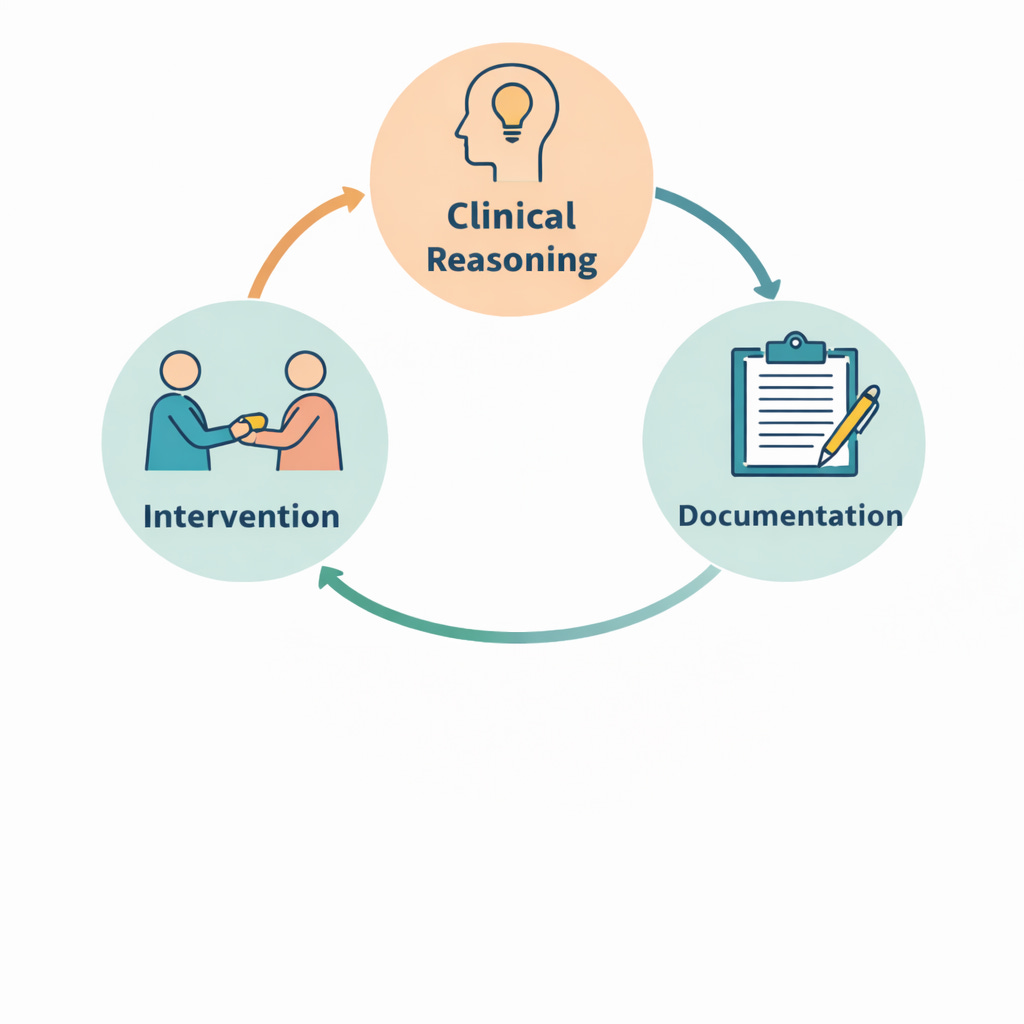
OT Practice Toolkit is built on the idea that treatment and documentation should be developed together. Clinical reasoning guides intervention. Intervention guides documentation. Documentation then reinforces clinical reasoning. When these pieces work as a single process, both treatment planning and note-writing become more intentional and more efficient.
This publication focuses on helping OT students and clinicians strengthen that connection—so treatment decisions make sense on paper, and documentation clearly supports skilled practice. Future posts will explore how to think through intervention choices, how to connect those choices to documentation, and how to write notes that reflect clinical reasoning rather than just activity lists.
If treatment feels easier than documentation, or documentation feels disconnected from what you actually did in session, you are not alone. Strengthening the relationship between the two is one of the most important steps toward practicing with confidence and clarity.
Paid Subscriber CTA
Paid subscribers receive focused guidance on:
Treatment ideas that clearly connect to documentation
Strategies for writing defensible, meaningful clinical notes
Clinical reasoning support for intervention planning
Upgrade to a paid subscription to access in-depth guidance designed for real-world OT practice.